Ear Infection – Earaches Ear Problems
While Scuba Diving
Adults and Children
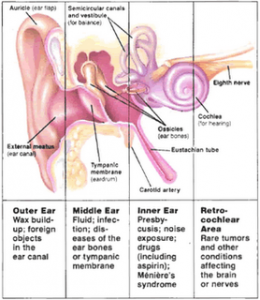
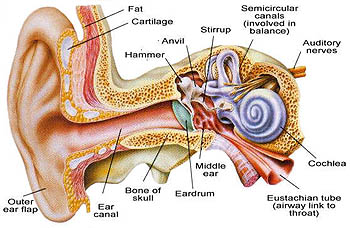
Diving Ear Infection are caused by either a bacterial or fungal infection of the outer ear infections or a viral or bacterial ear infection of the middle ear infections. Padi Diving Courses, swimming pools or even air conditioning will and can contribute to a Diving Ear Infection. Humidity, moisture, water can inhibit the growth of bacteria and infection in your ears. The outer ear is the visible part of the ear plus the ear canal, a small passage that conducts sound waves from the outside to the middle ear. The middle ear is a group of structures that include the eardrum and three small bones called ossicles that convey sound energy from the ear canal to the structures of the inner ear.
The middle ear is connected to the upper throat by a passageway called the Eustachian tube, which has two major functions: to equalize air pressure between the middle ear and the air outside the body and to drain fluid or mucus from the middle ear into the throat.
Ear Infection and Diving (Otitis Media)
Ear infection is common in children and adults, but can occur at any age. The main Symptoms of Ear Infections are earache and feeling unwell. Painkillers are the main treatment and Antibiotics are not usually needed but are prescribed in some cases. The infection usually clears within a few days depending on the infection.
Ear Infection and Diving (Otitis Externa)
An inflammation or infection of the ear canal. Any water entering the ear canal can increase the risk of the disorder. Diabetics are at increased risk. A middle ear infection that causes a ruptured ear drum can cause an otitis externa. Otitis externa is also called swimmer’s ear.
What is an ear infection?
An ear infection means that the middle ear is infected. The middle ear is the eardrum and the small space behind the eardrum. An ear infection is sometimes called ‘acute otitis media’. ‘Otitis Externa’ which deals with infection of the ear canal.
Infection of the outer ear is common. In the United States, it is more common in the summer months and in the warmer and more humid parts of the country and is more likely to affect adolescents and young adults than very young children.
Ear Infection of the middle ear, however, is much more common in young children than in older children or adults. There are two reasons for this. First, the immune systems of young children are less well developed than those of older children; second, the Eustachian tubes in young children enter the upper throat at a lower angle than in older humans. This difference makes it easier for disease organisms to stay in the tubes and cause inflammation and swelling rather than being carried downward into the throat.
Ear Infection of the middle ear are very common in children between six months and three years of age. According to the National Institutes of Health (NIH), 50 percent of all children in the United States have at least one episode of otitis media by the time they are a year old, and 80 percent have an episode by three years of age. The costs of treating these infection and their complications come to $4 billion each year. Otitis media is more common in the fall and winter months in the United States. It is somewhat more common in boys than in girls and is more common in Native Americans than in children of other racial groups. The reasons for these differences are not known.
Causes and Symptoms
Ear infection are caused by disease organisms causing tissue inflammation and fluid buildup in the skin of the outer ear or the structures of the middle ear. The symptoms of otitis externa may include:
- Sudden onset of pain
- Intense pain when the outer ear is pulled or moved
- Itching
- Swelling of the outer ear or nearby lymph nodes in the neck
- Feeling of fullness in the ear
- Temporary loss of hearing or feeling that sounds are muffled
- Pus draining from the ear
- The symptoms of otitis media may include:
- Red or flaky skin on the outside of the ear
- Intense crying in very young children
- Tugging or pulling at the ear
- Fever
- Irritability and headaches
- Trouble sleeping or poor feeding
- Nausea and vomiting (in small infants)
- Hearing loss
- Ringing or buzzing sounds in the ear
- the eardrum has ruptured
If the child has otitis media with effusion, there may be a slight hearing loss or no symptoms at all.
Diagnosis
The diagnosis of an ear infection is based on a combination of the patient Otitis externa can usually be diagnosed by simple movement of the outer ear, which will typically produce intense pain. When the doctor looks into the ear with an otoscope, the ear canal will look red and swollen, and there may be pus present. The doctor may take a sample of the pus or fluid and send it to a laboratory for culture. In the case of otitis media, the doctor will use a pneumatic otoscope to examine the child puff a small amount of air into the middle ear to see whether there is fluid behind the eardrum. If fluid is present, the eardrum will not move.
Another test known as tympanometry may also be done to measure the movement of the eardrum. In tympanometry, a small plug is inserted into the outer ear and air is blown into the ear canal to evaluate the movement of the eardrum. If there is evidence of hearing loss, the child may be referred to an audiologist for hearing tests.
How does an ear infection occur?
The small space behind the eardrum in the middle ear is normally filled with air. It is connected to the back of the throat by a tiny channel called the Eustachian tube.
The middle ear space sometimes becomes filled with mucus (fluid), often during a cold. The mucus may then become infected by bacteria or viruses. Children with glue ear who have mucus behind their eardrum are more prone to ear infections. Sometimes an ear infection occurs ‘out of the blue’ for no apparent reason.
What are the symptoms of an ear infection?
- Earache is common, but does not always occur.
- Dulled hearing may develop for a few days.
- Fever (high temperature) is common.
- Children may feel sick or vomit, and can be generally unwell.
- Young babies cannot point to their pain. One of the causes of a hot, irritable, crying baby is an ear infection.
- Sometimes the eardrum perforates (bursts). This lets out infected mucus and the ear becomes runny for a few days. As the pain of earache is due to a tense eardrum, a burst eardrum often relieves the pain. A perforated eardrum usually heals within a few weeks after the infection clears.
 About Earache:
About Earache:
Earache is a common symptom of ear infection. However, not all earaches are caused by an ear infection. If a child has earache but is otherwise well, an ear infection is unlikely. A common cause of mild earache is a build up mucus in the middle ear after a cold. This usually clears in a few days. Sometimes pain that you can feel in the ear is due to ‘referred pain’ from other causes such as teeth problems.
What is the treatment for an ear infection?
Most bouts of ear infection will clear on their own without treatment within 2-3 days. The immune system can usually clear bacteria or viruses that cause ear infections. However, treatments that may be advised include the following:
Painkillers
If the ear infection is causing pain, then give painkillers to children regularly until the pain eases. For example, paracetamol (Calpol, Disprol, etc) or ibuprofen. These drugs will also lower a raised temperature which can make a child feel better. If antibiotics are prescribed (see below), you should still give the painkiller as well until the pain eases.
Recent research studies have found that a few drops of a local anaesthetic drug (lignocaine) placed into the ear may help to ease pain. Further studies are needed to clarify the use of this treatment. However, it seems logical, and may become more widely used over time, especially in children with severe ear pain.
Antibiotics – are prescribed in some cases only
Antibiotics are not advised in most cases. This is because in most cases the infection clears within 2-3 days on its own. Also, it is best not to take antibiotics unless needed, as side-effects such as diarrhoea or rash can sometimes be a problem. Antibiotics are more likely to be prescribed if:
- The child is under two years old (as the risk of complications is greater in babies).
- The infection is severe.
- The infection is not settling within 2-3 days.
- Complications develop.
Sometimes, it may be difficult to see a doctor again in 2-3 days if things do not improve – for example, over a weekend. In this situation a doctor may issue a prescription for an antibiotic with the advice to only use the prescription to get the antibiotic if the condition does not improve within 2-3 days.
Treatment
Medicines may include: ear drops containing antibiotics and steroids. The ear canal should be cleaned of drainage. Non-steroidal anti-inflammatory medications/NSAIDs (ibuprofen/Motrin or Advil, naproxen/Naprosyn) and pain medications such as acetaminophen (Tylenol).
What are the possible complications from an ear infection?
It is common for some mucus to remain behind the eardrum after the infection clears. This may cause dulled hearing for a while. This usually clears within a week or so, and hearing then returns to normal. Sometimes the mucus does not clear properly and ‘glue ear’ may develop. Hearing may then remain dulled. See a doctor if dulled hearing persists after an ear infection has gone.
If the eardrum perforates, then it usually heals over within a few weeks once the infection clears. In some cases the perforation remains long-term and may need treatment to fix it.
If a child is normally well, then the risk of other serious complications developing from an ear infection is small. Rarely, a serious infection of the bone behind the ear develops from an ear infection. This is called mastoiditis. Very rarely, the infection spreads deeper into the inner ear, brain or other nearby tissues. This can cause various symptoms that can affect the brain and nearby nerves. See a doctor if a child becomes more ill, does not improve over 2-3 days, or develops any symptoms that you are not sure about.
Will it happen again, and can it be prevented?
It is common for children to have two or more bouts of ear infection throughout childhood. In most cases, there is nothing you can do to prevent the infection from occurring. However, there is some evidence to suggest that an ear infection is less likely to develop:
- In breastfed children.
- In children who live in a smoke free home. Passive smoking of babies and children can increase the risk of developing ear infections, and various other problems.
- In babies and young children who do not use dummies. However, research studies have shown that the use of a dummy in young babies when getting off to sleep can reduce the risk of cot death. It is not clear how, but it seems to help. So, regarding dummies, consider using a dummy in babies up to 6-12 months old at the start of each episode of sleep. However if you breast feed, do not start to use a dummy until you are well established with breastfeeding. This is normally when the baby is about one month old. But note:
- Do not force a dummy on a baby who does not want one. If the dummy falls out when a baby is asleep, just leave it out.
- Never coat a dummy with anything such as sweet liquids or sugar.
- Clean and replace dummies regularly.
- It is best to just use a dummy to help a baby get to sleep, but not at other times.
- Consider stopping using a dummy when the baby is about 6-12 months old.
Occasionally, some children have recurring bouts of ear infections close together. If this occurs, a specialist may advise a long course of antibiotics to prevent further bouts occurring.
Prognosis
Infections of the outer ear usually clear up completely in about a week without long-term complications. In some cases, however, people develop a chronic infection of the outer ear that extends to inflammation of the surrounding skin. A few people, most often those with diabetes or a weakened immune system, may develop a severe infection of the bone and cartilage near the outer ear that can cause severe pain and spread to the brain. This rare but potentially life-threatening complication requires treatment with intravenous antibiotics and sometimes surgery.
Most cases of otitis media improve within two to three days and clear up completely in a week or two without complications. If fluid remains behind the eardrum for long periods of time, however, it may eventually cause hearing loss. Another possible complication of recurrent or untreated otitis media is the spread of infection into air cells called mastoids in the bones around the base of the skull, a condition known as mastoiditis.
Prevention
Infections of the outer ear can be prevented by using ear plugs when swimming, avoiding swimming in polluted water, drying the ears after swimming or showering, and avoiding the use of foreign objects to clean wax out of the ears. It is very easy to damage the skin of the ear canal in this way.
Infections of the middle ear can be prevented by keeping a child away from children with colds or upper respiratory infections; by not exposing the child to tobacco smoke; by feeding the child in an upright position; and by breastfeeding the child for the first six months of life. Some doctors also recommend giving the child Prevnar, a vaccine that protects against pneumonia and appears to reduce the risk of otitis media as well.
The Future Ear infections are likely to continue being common health problems in children and adolescents. Researchers are comparing the effectiveness of tube placement versus removal of the adenoids in treating otitis media. They are also studying the effectiveness of the pneumonia vaccine in preventing infections of the middle ear.
Occasionally, a specialist may advise the insertion of a grommet into the eardrum if ear infections are very frequent. This is the same treatment that is used to treat some cases of glue ear. A grommet is like a tiny pipe that helps to drain fluid out from the middle ear. Some research suggests that this may reduce the number of ear infections that occur. See separate leaflet called ‘Glue Ear – Grommets and Other Operations’ for more detail.
References
- Otitis media – acute, Clinical Knowledge Summaries (July 2009)
- The management of common infections in primary care, MeReC Bulletin, Vol 17, No 3, 2006
- Respiratory tract infections, NICE Clinical Guideline (July 2008); Prescribing of antibiotics for self-limiting respiratory tract infections in adults and children in primary care
- Bolt P, Barnett P, Babl FE, et al; Topical lignocaine for pain relief in acute otitis media: results of a double-blind placebo-controlled randomised trial. Arch Dis Child. 2008 Jan;93(1):40-4. [abstract]
- Glasziou PP, Del Mar CB, Sanders SL, et al; Antibiotics for acute otitis media in children. Cochrane Database Syst Rev. 2004;(1):CD000219. [abstract]
- Foxlee R, Johansson A, Wejfalk J, et al; Topical analgesia for acute otitis media. Cochrane Database Syst Rev. 2006 Jul 19;3:CD005657. [abstract]
- McDonald S, Langton Hewer CD, Nunez DA; Grommets (ventilation tubes) for recurrent acute otitis media in children. Cochrane Database Syst Rev. 2008 Oct 8;(4):CD004741. [abstract]
Dont Suffer with Ear Infection – Earaches From Diving
Learn More About Diving Professionals or Become a Padi Scuba Instructor with Easy Divers Cyprus